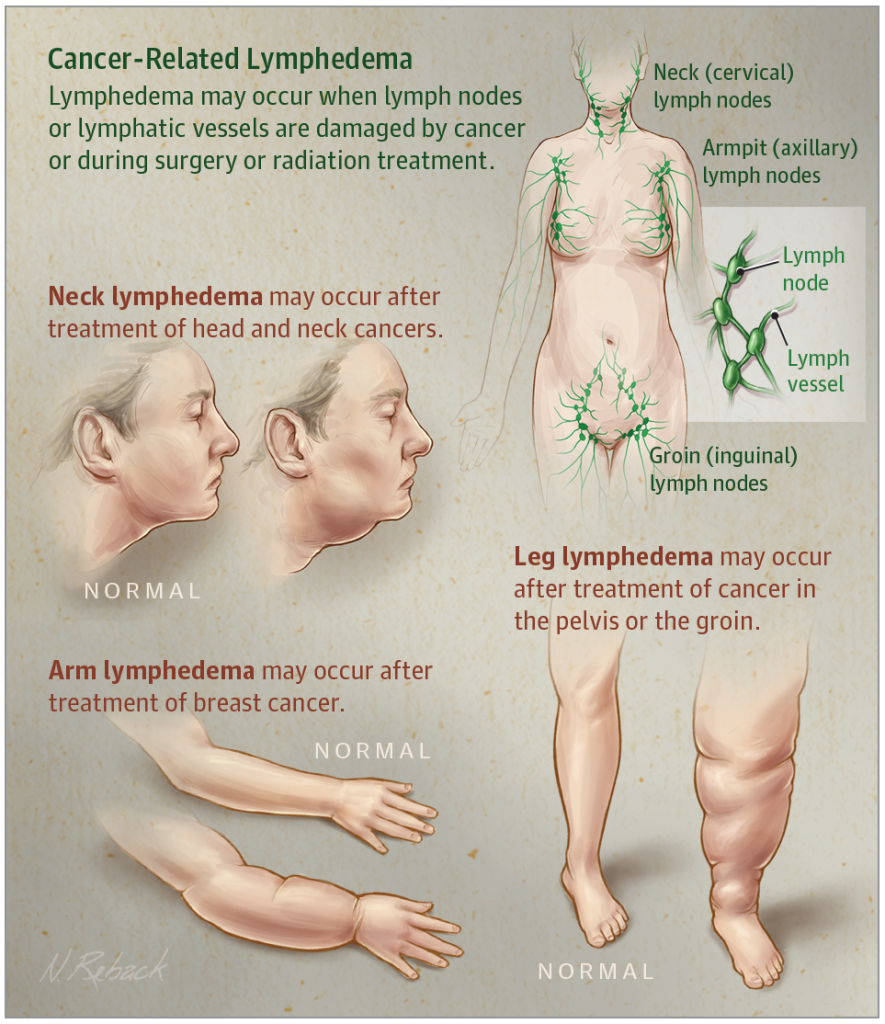
“Lymphedema is marked by chronic and sometimes painful swelling,” said Hari Kashyap, a certified lymphedema therapist working at the Georgia Cancer Center. “It occurs due to accumulation of lymph fluid in different areas of the body. Swelling most commonly occurs in the arms, legs, trunk, abdomen, head and neck, or external genitalia.”
Lymphedema may interfere with wound healing and increases the risk of infection. Those afflicted with swelling in the legs may experience difficulty walking. Swelling in the arm may result in a feeling of “heaviness” and it may be difficult to reach.
Augusta University Health’s Lymphedema Risk Reduction and Treatment Program is the most comprehensive and extensive in the region.
“Facial, neck, and intraoral swelling can affect swallowing, communication, and mobility,” Kashyap said. “Lymphedema can result in decreased quality of life due to restricted use of the affected body part.”
Lymphedema is categorized as either primary or secondary. Primary Lymphedema is caused by an abnormality in the lymphatic system which is present at birth or may occur later in life. Secondary Lymphedema is more common.
“It is often a side effect of cancer treatment, where lymph nodes are removed and can result in swelling due to blood clots, trauma, circulation problems and infection.”
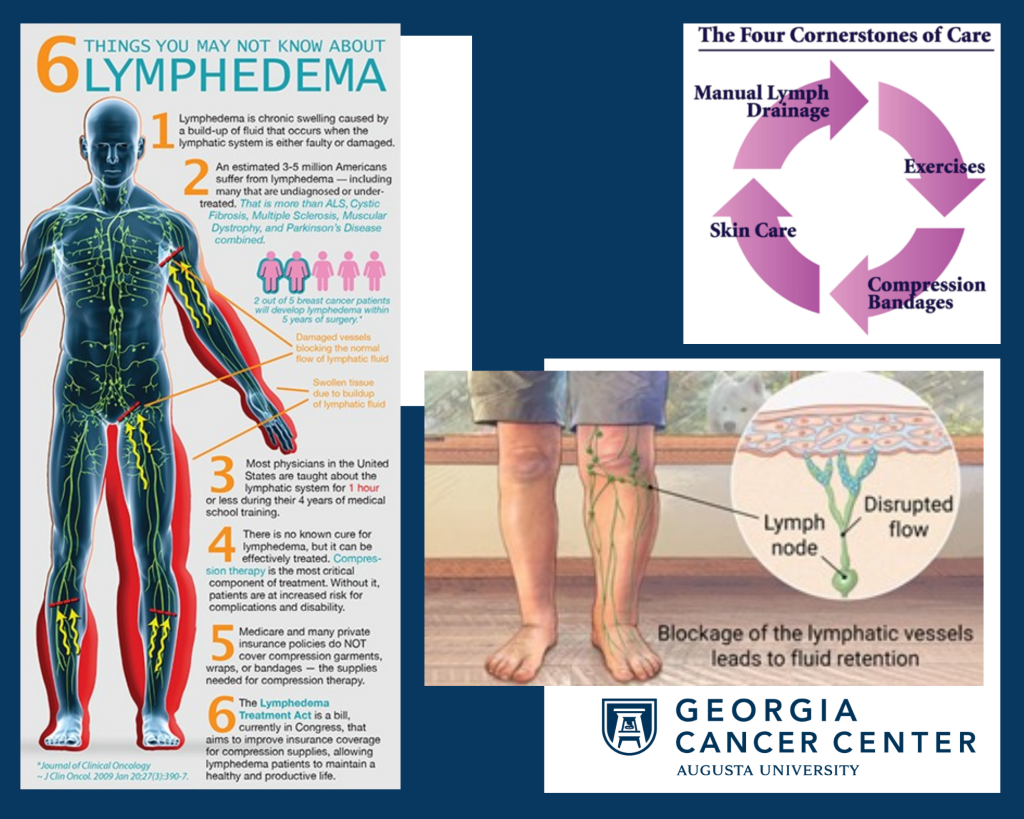
Steps can be taken to reduce the risk of lymphedema development. Healthy habits for patients at risk for lymphedema development include maintaining a healthy diet with plenty of exercise and finding a certified lymphedema therapist who can review your situation, prescribe compression garments and exercise as needed, screen for lymphedema, and discuss personal risk factors.
Augusta University Health’s Lymphedema Risk Reduction and Treatment Program is the most comprehensive and extensive in the region. Complete treatment and education empower patients to take control of their own recovery. Treatment provided by a nationally certified therapist at our Lymphedema Clinic includes:
- Comprehensive evaluation of each patient’s medical history, lymphedema, and functional limitations
- Lymphedema risk reduction education
- Manual lymphatic drainage
- Compression Bandaging
- Skin care program to prevent infection
- Exercise instruction
- Recommendation and fitting of compression garments
- Instruction/education for home program to build independence in self- management
- Pre-operative measurements to set baseline for those who meet criteria with continued follow up screenings to monitor for early development of Lymphedema
A physician referral or order is required for treatment at our Lymphedema Clinic and can be faxed to 706-721-1459 or called in to 706-721-2481.
“Most insurance plans and Medicare cover the cost for this service,” Kashyap said. “If you would like to be seen for this service, simply ask your physician or nurse to make a referral to the Lymphedema Clinic.”