It’s taken three years and several hospitalizations, but Dianne George finally knows what’s wrong with her heart, and it’s not one of the usual ailments.
She has sarcoidosis.
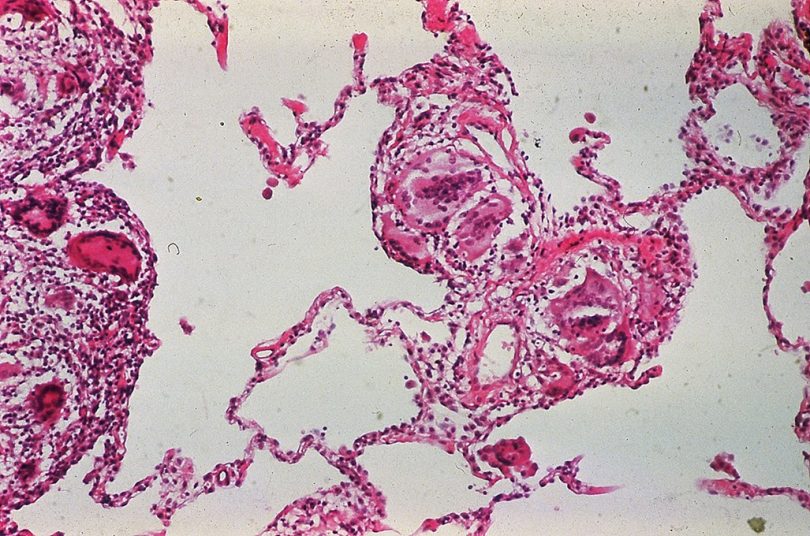
The condition is often missed partly because symptoms are not obvious, and partly because many physicians don’t know about it. Sarcoidosis is an inflammatory disease that causes clumps of immune cells, called granulomas, to form in tissues and organs.
“We don’t know what triggers it, and we don’t understand why certain people get it and are more susceptible to it,” said Dr. Neal Weintraub, Division Chief of Cardiology and Professor of Medicine at Augusta University’s Medical College of Georgia. “It’s most common in Blacks, and it’s also very common in Scandinavia.”
It can affect almost any organ, though the lungs are most commonly involved.
For George, the granulomas form in her heart. When symptoms involve the heart, the first symptom might be sudden death.
That’s one thing that makes George’s case unique: she’s here to tell her story.
“It all started in June of 2019,” she said. “I was a teacher, and I walked the neighborhood during the summer, in the morning. That summer, I started walking but I would get out of breath, dizzy and stuff.”
On her way to Edisto for a beach trip with her husband, she joked that at least she had never passed out.
“Probably 20 minutes later, after saying that, I passed out in the car,” George said. “Harry tried to find my pulse and he couldn’t find it. I recovered fairly quickly, but I didn’t feel right.”
They went to a nearby prompt care clinic, which sent her to a local hospital because while her blood pressure was good, her heart rate was off. She received a pacemaker and thought that solved her problems.
In November, she started having ventricular tachycardia – her heart was beating very fast and weakly. Her cardiologist in Aiken, where she lives, sent her to Wellstar MCG Health (formerly AU Health), where she was placed on medical therapy and her pacemaker was changed to a CRT-D device, which has a defibrillator that shocks the heart to restore a regular heartbeat rhythm.
George began receiving repeated shocks from her device and was readmitted the following month. Weintraub became involved in her care and almost immediately suspected the culprit could be sarcoidosis. He ordered several tests, including a PET scan and bronchoscopy with a biopsy, which confirmed the diagnosis.
He prescribed several medications designed to treat inflammation, as well as heart medications. The heart rhythm calmed down almost immediately and her heart function recovered.
Cardiac sarcoidosis can become very serious if the diagnosis is not made, Weintraub said. Besides dangerous arrhythmias, patients like George could present with heart failure, with no obvious cause such as blocked arteries to explain it, he said.
“The problem is a lot of physicians are not aware of cardiac sarcoidosis at all. Even many cardiologists don’t think about it. Since they don’t think about it, they can’t make the diagnosis,” he said. “If you have cardiac sarcoidosis and proper treatment is not given, the prognosis is dismal. Most people that have untreated cardiac sarcoidosis will be dead within a few years.”
Sarcoidosis is very common in the southeast, and that is one of the reasons Weintraub and his colleagues have established the sarcoidosis clinic at Wellstar MCG Health. Not only is the disease very serious with potentially life-threatening consequences and can be difficult to diagnose, but a diagnosis also typically requires advanced imaging capabilities that aren’t always available – especially in smaller communities.
“So we felt that here at Wellstar MCG Health, we were in exactly the right place and have the right people and resources to bring together to form this clinic so that we can serve the region,” Weintraub said.
When a patient comes to the clinic, they see a cardiologist, a pulmonologist and a rheumatologist who all have expertise in sarcoidosis. The cardiologist and pulmonologist help investigate problems with the heart and lungs, and the rheumatologist helps investigate problems with joints (another common site of involvement of the disease). The rheumatologist can also initiate medications that help suppress the immune system, which is an important part of treatment. The team will also refer to an ophthalmologist or dermatologist if eye or skin involvement is suspected. Protocols have been established to follow patients up and ensure that the inflammation is controlled, and medications are tightly monitored.
“The patient can come to one clinic and see three different physicians who all share their expertise and come up with the best plan for diagnosis, treatment and followup,” Weintraub said.
George credits Weintraub and the rest of her care team for her ability to continue to be involved in the things she enjoys, although in a more limited capacity. She continues to travel with her husband, care for her granddaughters and be active in her church through careful management of her symptoms.
“And I can share my story,” she said. “It’s not a death sentence, by any stretch of the imagination. You just have go to about things in a little different way.”
Wellstar MCG Health recently joined 42 other institutions as a member of the Foundation for Sarcoidosis Research Global Sarcoidosis Clinic Alliance.