Doctors at Augusta University Health are introducing innovative programs to provide quality care to as many patients as possible. One of those programs allows patients to have 24/7 care and reduces cost, all from the comfort of their own home.
AU Health’s Virtual Care at Home program is designed to aid the rest of the hospital with increased bed capacity. The hospital is the only one in the state of Georgia with this type of individualized care, which has treated patients dealing with anything from COVID-19, pneumonia, heart failure, cellulitis, and asthma.
Lauren Hopkins, AVP of Virtual Care & Community Engagement at AU Health, said the program started in February 2021, when beds in the hospital were virtually unavailable during the COVID-19 pandemic. The Virtual Care At Home program allows the AU Health Care team to discharge patients from the hospital earlier while continuing to provide around-the-clock monitoring of vital signs through remote monitoring. Patients will receive a daily virtual visit with an AU Health provider.
“These patients do not need care in a skilled nursing facility or rehab center, but they do need a more robust transitions of care program to help avoid a readmission or ER visit,” said Hopkins. “This program also helps identify patients who may not necessarily need to be admitted. We can enroll patients from the Emergency Department into this program, which helps the patient save money and helps reduce the number of patients in the ER waiting room.”
The program is available to AU Health patients, who have ranged in age from 12 to 90. Once they are enrolled in the program, a remote monitoring kit is given for the patient to bring home with them.
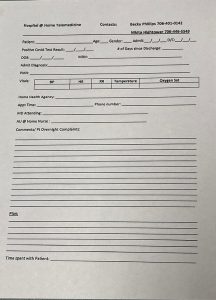
These kits monitor temperature, blood pressure, pulse oximetry, and other vitals depending on the patient and their condition. The patient does not need Wi-Fi to participate as the kit and virtual visit can work off a cellular network.
If a patient’s blood pressure is elevated or a problem arises, the nursing staff escalates to the on-call medical provider, who visits the patient virtually and review their vital signs and symptoms. If the patient needs to be sent back to the Emergency Department, medical staff will coordinate with the patient and their family to have the patient come back to AU Health for a higher level of care.
Dr. Matthew Lyon, Service Chief for Virtual Care at AU Health, said, “The service is customized for the individual need. The program does not provide advanced imaging or other intense needs that would be done in the hospital. It is a transitional bridge for patients who need to be discharged but still need some help from nurses, nurse practitioners and physician assistants.”
Another factor for the program is the environment around the patients. These patients can be high-complexity or low-complexity cases, which would change the number of check-ins and vital readings from hospital staff. The plan around each patient can be managed on a case-by-case basis, working around the patients’ needs to make sure the program works for them.
“Enrollment is diagnosis-specific, but the plan around the patient is developed based on all types of factors,” said Lyon. “It’s looking at the patient’s environment: do they have other family members taking care of them or are they a patient that’s less independent? That’s what I think is the best part of this.”
Hopkins said the response from patients in the program is positive. They appreciate the personal feel and one-on-one consistency with the nursing staff and providers. So far, the virtual care team has treated more than 570 patients, totaling over 3,500 patient days. Readmission rates for patients back to AU Health are less than 7%. This program also helps the hospital save six inpatient beds per day. This is extremely critical when hospital capacity is still high.
“There is a lot of new technology to create innovative ways to deliver care through digital means,” said Hopkins. “This is a new way and avenue that allows us to go from ‘No, we cannot do it’ to ‘How can we do this?’”
Lyon pointed to the training involved with new telehealth programs as a main reason for its success. During the pandemic, leaders in the telehealth field focused on the need for training and education with providers and how to incorporate telehealth into their practice.
The Medical College of Georgia now has curriculum for residents, students, or providers to hone their skills.
“It’s easy to think talking one-on-one like FaceTime is telehealth, but it’s so much more,” said Lyon. “There can be pitfalls that are not immediately obvious if you do not receive training on how you can really use this platform to enhance your practice and provide high, quality healthcare.”